Chew Valley Listening Project results are in
Community First carried out 125 listenings with residents in Chew Valley between January-March 2024. Community Organisers listened to people in six neighbourhood communities and two community groups.
Background
In partnership with Community First, we undertook a listening project within the Chew Valley community to better understand what is felt to be important locally in terms of life-limiting illness. This covered what support is needed to both live well and die well and support with associated loss and bereavement.

For Dorothy House, growing our understanding of our community’s aspirations for end of life care is important. Having recently succeeded St Peter’s Hospice in providing clinical care in the area, we wanted to hear from the local residents regarding what they feel their area wants and needs.
As well as on our 10-bed Inpatient Unit, we offer care in people’s own homes through a dedicated local team. However, this can only ever meet part of what matters most to people at the end of their lives.
Our mission is that everyone has access to outstanding palliative and end of life care, fully acknowledging the vast amount of end of life care that is provided by local services, neighbours and loved ones. We can only achieve that mission together.
Community First is an early adopter of Community Organising techniques. They adopt this approach in an open and effective way to meet and talk to local people on matters that are important to them. It is the first step in seeking to understand what can be achieved by building on the strengths that already exist in communities.

Demographics
- Overall, more female (66%) than male (33%) residents took part in listening activity.
- Over 80% of all residents were over the age of 45 years, with the highest percentage of listenings carried out with those in the 45-54 (19%) and 75-84 (22%) age categories.
- Amongst residents aged 35-44 and 65-74, the balance of male and female listenings was closer to equal when compared to other age ranges.
Experiences of Life-Limiting Illness
- Almost three-quarters (74%) of the residents who took part in the listening activity had an experience to share around life-limiting illness. Amongst these residents 82% had previously cared for a person who died, 12% are currently caring for someone and 6% are currently living with a life-limiting illness.
- 35% of residents who had experience of life-limiting illness provided care for or are currently caring for a parent or in-law, 24% for a spouse and 10% for another family member.
- Support is/was received from friends and family members (42%), healthcare providers (42%), private carers (34%) and a hospice (29%). 40% of residents stated they were/are the main carer.
- 30% had a positive experience of support, with 20% who felt their experience was negative.
Positive factors included hospice care, NHS care and support from charities. Negative factors included feeling let down by NHS services and coordination and standard of care. - Some residents said their loved one received good care towards the end of their life, but that their own experience of being a carer was fraught and difficult. Some carers suggested they felt forgotten about or unable to access the support they needed at the time they were caring for a loved one.
- 33% of residents said additional support would have been helpful. This included respite care, bereavement support and practical support.
“A system where the care services join up the dots – better signposting, because when you are in this overwhelming situation you can’t think straight and need support and advice not constant obstacles.”
Local Support for Life-Limiting Illness
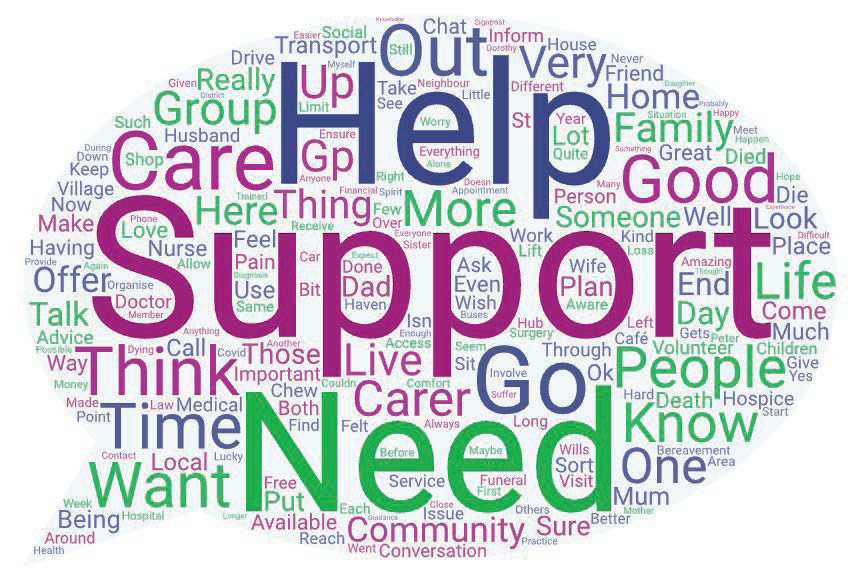
- As part of the listening activity, residents were asked what support is felt to be important locally.
- Themes included health and care services, communication and signposting, practical support, emotional support (including bereavement) and community groups. A detailed analysis of each of these themes is explored in the report.“I think you need a good team of carers, but the same carers need to be seeing the same patient. They need continuity and so do the family. You can’t build any sort of relationship if you see someone different daily…”

Thinking about and planning for end of life
- Over half (55%) of residents had previously had a conversation about planning for the end of their life. 28% said they had not had a conversation.
- Amongst those who had made plans, these included a will, Do Not Resuscitate (DNR) request, living will, power of attorney or funeral arrangements.
- Comfort, dignity and peace were the most common themes amongst people asked what matters to them when they think about the end of their life. People would like their death to be quick and as pain free as possible, with family members and loved ones around them.
- Some individuals said they would like to die in their own home, others said they would like to die in a hospice with the support of hospice staff.
- There were several comments from residents in favour of assisted dying. These individuals suggested people should have the right to choose when they die.
“We have had conversations. We have made wills, and our wishes are known. I want to be cremated and kept in a box. It’s important to me that the family are all ok and are taken care of. I think it is easier for the children if those sorts of conversations have been had.”
Life-Limiting Illness – Community Support
- Over three quarters (77%) of residents indicated support from the wider community was important for people affected by life-limiting illness, with 9% who felt it was not an important factor.
- Despite this, the percentage of Chew Valley residents who suggested they were satisfied with
the level of community support or community spirit in their own community was lower overall at 28%. - There were geographical differences in sentiment towards the level of community support and community spirit in different communities in the Chew Valley area. Residents who attended community groups had higher satisfaction overall.
- Amongst the villages, Chew Magna, Clutton and Chew Stoke had the highest satisfaction level. Bishop Sutton, West Harptree and Temple Cloud had a lower level of satisfaction with community support and community spirit.
- Perception of community support was also (to some extent) age dependent, with older residents reporting a better experience of community support compared to younger residents.
- Groups and organisations like the Death Café, Chew Chat and the widows group were important sources of community support for some residents. Village Agents and Good Neighbour services were also felt to offer a means of practical and emotional support for people affected by life-limiting illness.
- Some residents were not in favour of community support for life-limiting illness and felt it was inappropriate. This was due to the complex nature of life-limiting illness (and the need for support and training), as well as a feeling that volunteers may be expected to do too much for the community.
“Someone to support you through those tricky times, to share the ups and downs through the progression of the illness. Someone to help you prepare for what is to come. Some support when your loved one is no longer here. That’s something I find very hard now 2 years on and it’s hard to find people that can relate. Friends are amazing but can only relate on an emotional level, not an intellectual one as they haven’t all experienced what I have.”
Resources for the Community
- Residents were keen to share their ideas for resources which could help support members of the community who want to help people affected by life-limiting illness.
- Key themes included transport, increased resources e.g. additional volunteers and support for local groups and improved signposting to knowledge and information. A deeper analysis of these themes is explored in the report.
“The Death Café. Somewhere like this has been so beneficial to me and I think would be a great source of comfort for many others…”
Recommendations
A range of recommendations for next steps are presented in the full report. These include a palliative and end-of-life care information hub, offering practical and emotional support to carers by building on existing volunteer and community group capacity, developing a community-transport offer for people affected by life-limiting illness in Chew Valley and community mapping to develop a complete picture of support, services and gaps locally.
We are already evaluating these recommendations and look forward to working with our community partners to explore options. We will be sharing details of further community events with you shortly.
To access the full report Dorothy House Hospice Care – Chew Valley Listening and Engagement Project Report, click here.
- Share this page:
- https://www.dorothyhouse.org.uk/?p=134959
